Optimizing Nutrition When Coming Off The Pill
Birth control, or the pill, is taken by about 21.6% of women 20-29 years old.
Women are put on birth control for a variety of reasons: preventing pregnancy, PCOS, acne, irregular periods, absence of periods, uncontrollable cramps, PMS symptoms, and moodiness just to name a few. Regardless of your reason for wanting to stop the pill, supporting this transition and shift in hormones by optimizing nutrition and lifestyle is critical in successfully returning to your natural menstrual cycle.
How does birth control impact the body and menstrual cycle?
While there are a variety of different types of birth control pills on the market, they all share a similar mechanism to preventing pregnancy. Progesterone, a hormone that is responsible for preventing pregnancy, is taken daily in pill form. When your body recognizes an increase in progesterone, follicular growth is halted. Typically, follicular growth helps ovarian follicles develop and mature, leading to ovulation. However, on birth control, ovulation is prevented, meaning a mature egg is not released from the ovaries.
Some birth control pills also contain estrogen. Estrogen also inhibits follicular development and controls menstrual bleeding. The hormone acts on the uterine lining by thickening it and promoting blood clotting.
Pills that contain both estrogen and progesterone are considered combined oral contraceptives, and are the most commonly prescribed form of birth control.
The period you get on birth control is not the same as a natural menstrual period. Your time of the month on birth control is caused by a drop in hormones, either progesterone or progesterone and estrogen based on your pill formulation. This bleeding is referred to as “withdrawal bleeding” due to ingestion of inactive pills containing no hormones. It is common for your “period” on birth control to be much lighter for this reason.
Why might someone consider getting off the pill?
Just like there’s many reasons why someone gets on birth control, there are just as many reasons why someone may want to quit birth control. These include:
Trying to conceive
Negative side effects on the pill (nausea, headaches, mood, weight, and libido changes, etc.)
Interest in shifting to non-hormonal birth control methods
RED-S (Relative Energy Deficiency in Sport)
Natural regulation of period
What happens to your body when getting off the pill?
When taking birth control, your body’s natural estrogen and progesterone production stops to override your natural cycle and prevent pregnancy. When you stop taking pills containing progesterone and/or estrogen, your body tends to react by displaying common symptoms. Some common symptoms post birth control include:
Acne
Irregular periods
Absence of periods
Hair loss
Mood swings
Physical body changes
Changes in gut and liver function
Nutrient depletions
What changes can I make to my nutrition and lifestyle to support this transition?
Before quitting birth control, consult your healthcare team to see what the best plan is for you. If you get the green light, these are recommended changes that you should make before officially quitting the pill to reduce common side effects, support your body’s changing needs, and return to a natural monthly cycle.
Eat enough calories
Consuming enough calories to meet your energy needs is a key component to rebalancing your hormones. This helps to support ovulation, as well as natural production of estrogen and progesterone hormones. In particular, focusing on eating more healthy fat sources, including olive oil, avocado oil, fatty fish, nuts, seeds, and avocados can be beneficial.
Additionally, foods considered phytoestrogens, or plants that mimic estrogen in the body, can have positive impacts during this transition. Foods containing phytoestrogens include beans, legumes, flaxseeds, whole grains, berries, and cruciferous vegetables. Focus on consuming a well-balanced diet with sufficient fat and added phytoestrogens to help return to your natural cycle.
Replenish nutrient deficiencies
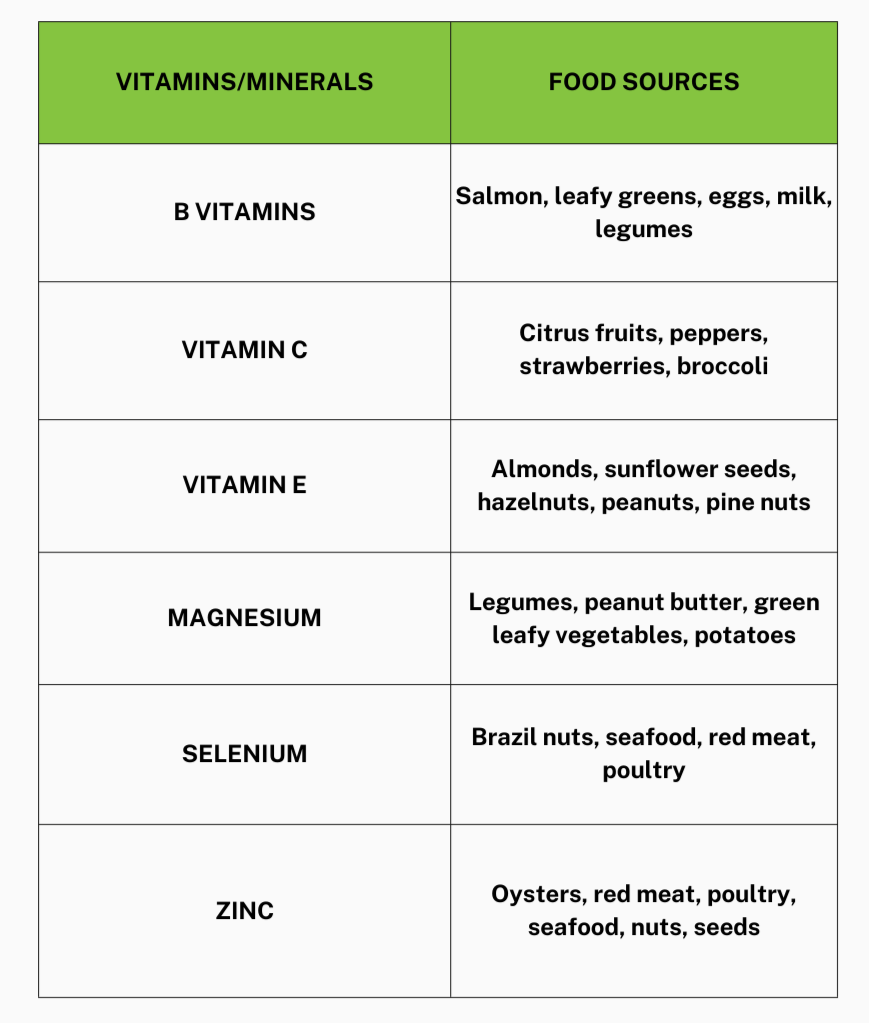
Women taking birth control require differing amounts of vitamins and minerals than women who are not on the pill. Birth control can deplete your body’s levels of B vitamins, vitamin C, vitamin E, magnesium, selenium, and zinc.
Getting your labs drawn before getting off the pill can be helpful to better understand your nutrient needs and what vitamins and minerals you may need to focus on increasing in the diet. Correcting abnormal labs before getting off birth control is beneficial in supporting your body during this shift in hormone levels.
Improve gut health
Birth control has been found to cause a decrease in gut microbiome diversity, meaning that there is a smaller amount of variety in the microorganisms living in the gut. Foods rich in prebiotics, probiotics, and foods that are fermented can help to increase the good bacteria in your gut. Consuming plenty of fruits, vegetables, whole grains, legumes, and dairy can aid in improving your overall gut health.
If you regularly experience abnormal bowel movements or gastrointestinal distress (abdominal pain, bloating, nausea, vomiting, diarrhea, constipation), getting a GI-MAP (Gastrointestinal Microbial Assay Plus) test before getting off the pill may be beneficial for you. This test allows your provider to understand your personal gut makeup and they are able to create a plan to personalize your nutrition to improve your specific gut microbiome.
Lifestyle changes
Making intentional lifestyle changes can support your body as you transition off birth control. Reduced physical activity, lower stress levels, and quality sleep all play a role during this period. While staying active is essential for overall health, it’s equally important to prioritize rest. Focus on gentle movement, such as walking, yoga, and moderate resistance training.
Managing stress and prioritizing quality sleep are also vital for restoring natural hormone production. Aim for 7-9 hours of restful sleep each night and maintain a consistent sleep schedule. Elevated stress can increase cortisol levels, negatively impacting your menstrual cycle and even interfering with ovulation. Explore stress management techniques that align with your lifestyle to help prevent these issues and promote hormonal balance.
When would it be necessary to meet with my Physician or Dietitian after getting off the pill?
After you stop taking birth control, it is important to continue to follow up with your healthcare team to monitor your return to a natural menstrual cycle. If your symptoms begin worsening or your period hasn’t returned after 3-6 months, reach out to your care team to determine the best plan of action for you. Working with a dietitian while getting off birth control can be beneficial to better understand your personal dietary needs and recommendations.
The bottom line:
While transitioning off of birth control can be overwhelming, optimizing your nutrition before finishing your last pack is key to smoothly transitioning off the pill. Be patient and gentle with yourself throughout the process and understand that there may be some unpleasant symptoms that arise, but with these recommendations, getting back to a regular cycle is possible.
Feeling intimidated and nervous to finally say goodbye to birth control? Schedule an initial consultation today to discuss how we can help you develop a personalized care plan to make the transition as smooth as possible!
Learn more about how birth control impacts athletes on our Instagram!
References:
Daniels K, Abma J. Current contraceptive status among women aged 15-49: United States, 2017-2019. Centers for Disease Control and Prevention. October 20, 2020. Accessed July 12, 2025. https://www.cdc.gov/nchs/products/databriefs/db388.htm
Cooper DB, Patel P. Oral contraceptive pills. [Updated 2024 Feb 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430882/
Palmery M, Saraceno A, Vaiarelli A, Carlomagno G. Oral contraceptives and changes in nutritional requirements. Eur Rev Med Pharmacol Sci. 2013;17(13):1804-1813
Mihajlovic J, Leutner M, Hausmann B, et al. Combined hormonal contraceptives are associated with minor changes in composition and diversity in gut microbiota of healthy women. Environ Microbiol. 2021;23(6):3037-3047. doi:10.1111/1462-2920.15517